Lupus and the Microbiome: What Is Your Gut Telling You?
A quickly growing amount of research has been devoted to seeing how lupus is affected by gut health, not only in how the disease can be helped by good bacteria, but how it might even be triggered by bad ones!
- Introduction
- The Amazing World of Your Internal Ecosystem!
- Could Gut Bacteria “Cause” Lupus?
- Keeping Your Gut Healthy and Bacteria Happy
- Dr. Teri Greiling on Lupus and the Microbiome
- In Conclusion
Introduction
Estimates vary, but it is likely that there are from 38 to 100 trillion bacteria in each of our digestive tracts right now – more than all of the stars in the Milky Way galaxy (~300 billion). That is also more, possibly A LOT more than all of your own human cells in the rest of your body. Quite simply each of us is outnumbered by our microbial guests, and we are more dependent upon them than we might like to think.
It has been clear for some time now that when these microbial communities are stable and in good health, we tend to also be in good health. Conversely, when the intestinal community is out of balance, it can have dramatic effects on our health – not just digestive health, but also health issues that would seem totally unrelated. In particular, this is increasingly the case for autoimmune diseases like inflammatory bowel disease, fibromyalgia and possibly lupus.
.
The Amazing World of Your Internal Ecosystem!
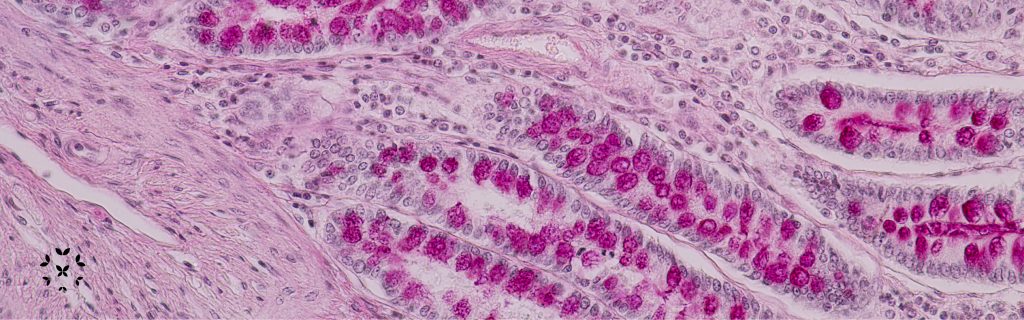
The internal collection of microbial life is called our “normal flora.” It is also called the “microbiome,” because it exists as a microscopic ecosystem of tiny interacting species – including predators and prey – that can resemble the earth’s macro-biomes, such as forests or desert communities.
Some fun facts about this internal community:
- Not everyone has the same natural flora. Europeans and Americans generally have fewer species of bacteria in their guts than those in less industrialized countries. This is most likely due to differences in diets and sanitation. This may at first seem like a good thing for the industrialized person, but not necessarily. The overuse of antibiotics and processed foods reduces the diversity of these microbiomes, and that can have negative consequences.
- Lupus patients have a different mix of oral/mouth bacteria than those without SLE. A 2023 study compared the mix of oral bacteria in patients with SLE and found that not only do those living with lupus have a distinctive and more diverse collection of bacteria compared to those without lupus, but also the mix of bacteria changes depending upon the level of lupus disease activity. This finding may lead to a better understanding of the connect between lupus a person’s natural microbiome; it may also lead to an easier and non-invasive way for physicians to both identify lupus and measure the effectiveness of treatment plans!
- Where did our first bacterial partners come from? We all normally start off with no bacteria or other types of organism in our digestive systems. In the uterus, we ingest amniotic fluid as we develop. That is usually a sterile environment, however, the process of birth changes things dramatically. Most babies in the world, and throughout history, are/were born by passing through the birth canal. If you did so, you were completely covered by the microbes that lived along the walls of your mother’s birth canal and you became inoculated with millions of them. As you ingested them – you really couldn’t avoid it – they were the first to populate and influence your digestive system.
- Natural versus Cesarean Births: Babies delivered by Cesarean do not get the benefits of the mother’s s birth canal microbes. That means bacteria from medical staff, equipment and even the hospital room get to the baby’s digestive tract instead. Studies have shown that this could affect the immune system and may lead to higher rates of food allergies or asthma. Just in case, some hospitals now swab the birth canal of mothers at the time of birth and inoculate the face of the newborn with these beneficial microbes. The effects on autoimmune diseases, such as lupus, have not yet been documented.
- Mother’s milk is usually the first food that any of us get after we are born. So, the nutrients and the bacteria that are a natural part of breast milk have evolved to be appropriate for the baby and can have a huge effect on a her natural flora and immune system.
- Bacterial Cures? Some microbes can stimulate the human immune response in ways that are beneficial for us … and them. Several are being studied to see if they can actually prevent or treat disease. For example, research has shown that a species called Bacteroides fragilis can help reduce the painful inflammation of colitis. This may have the potential for the treatment of lupus as we will see later in this article.
- Fecal Transplants: It has also been shown that transferring gut bacteria from a healthy person to someone who is sick with antibiotic-resistant Clostridium difficile, can actually cure that disease. There have even been other studies to see if fecal transplants can help patients with autism.
- Microbes on the Brain? Both the brain and the digestive system send chemical signals to each other through the circulatory system. Microbes in the gut can induce cells of the GI tract to send hormones to the brain. Believe it or not, 80% of your body’s serotonin (a neurotransmitter that affects mood, sleep and memory) is produced in the gut, not the brain!
Could Gut Bacteria “Cause” Lupus?
The critical role of gut bacteria has been well documented for disorders of the digestive system, like irritable bowel syndrome (IBS) and chronic dysfunctional pelvic pain. However, gut health has only been recently found to be associated with either affecting or perhaps even causing lupus and other autoimmune diseases. This area of research is changing quickly; here are some of the latest findings:
In 2018, researchers found that a gut bacteria, Enterococcus gallinarum, could escape the digestive tract to the blood stream and then to the liver and lymph nodes where it could hide out for years, and possibly trigger an autoimmune response.
In 2019, a study of 61 women with lupus found that another type of intestinal bacteria, Ruminococcus gnavus, existed in much higher levels (approximately 5 times higher) compared to women without lupus. What is more, the amount of this bacteria increased with the onset of lupus flares and decreased in times of remission. Blood tests from these patients also saw elevated antibodies to the bacteria in proportion to the severity of the flare. This was most pronounced with kidney flares. How? Here are some clues:
- The increase in antibodies suggests that somehow these bacteria (or pieces of these bacteria) leak from the intestines and make their way through the blood stream. “Leaky gut” or altered intestinal permeability is a theory that is quickly gaining attention in the medical community.
- These bacteria, then, may trigger an immune response that turns into an autoimmune response. The antibodies used to attack R. gnavus seem to be the ones that attack the DNA of lupus patients. Could this be similar to how a certain type of streptococcus bacteria can trigger the autoimmune antibodies that cause rheumatic fever? Well, more research needs to be done.
It is important to understand that this, so far, is a correlation between R. gnavus and E. gallinarum and lupus, not causation. Meaning, it is unclear whether the bacteria causes the flare, or the flare causes an increase in the bacteria, but it is probably a relationship that works both ways. Even if this particular bacterium is not a definitive cause for lupus, the presence of its antibodies could give physicians an easier blood test for diagnosing lupus than we have currently and provide a better way to measure the severity of flares.
Another 2019 study has shown that a strain of bacteria, called Lactobacillus reuteri, was found in greater abundance in the microbiomes of SLE patients. These bacteria were also found to make their way to the blood stream and end up in patient lymph nodes, liver and spleen. This is thought to trigger an autoimmune response by increasing the production of Type I interferons, which in turn drives many of the problems associated with lupus.
It was later found, in 2022, that both E. gallinarum and L. reuteri could actually undergo what is called “within-host evolution” in order to gain this ability and that they might evolve differently in different people. What does this mean? It could explain why lupus expresses so differently in those living with it – and this insight may lead to more individualized treatments for each patient!
Again, this is still the very beginning of this research, and no one is calling for changes to the current treatment options. Always consult your healthcare practitioner regarding your own treatment options.
.
Keeping Your Gut Healthy and Bacteria Happy
Remember, you are eating for trillions! When you eat, you are not just ingesting nutrients for yourself, you are feeding all of your closest microbial friends. If you want to keep them in a good mood and keep the unfriendly ones out, think about the food that is best for them as well as you. Diets that support a healthy microbiome include:
- Lots of vegetables and whole grains, though some may not fit an autoimmune diet.
- High quality protein, like fish and legumes, with limited amounts of red meat.
- Fermented dairy and vegetable foods, like sauerkraut, yogurt, kefir, and kimchi.
- None or limited amounts of refined carbohydrates and sugars.
Probiotics are also an option. They have become a popular diet supplement for many, and it is estimated to be a roughly $50 billion global industry. Probiotics come in many forms, and their quality and price can vary considerably. They generally contain a mixture of bacteria and yeast strains that are said to establish a healthier community of organisms in the digestive tract. There are many studies that show how some probiotics can reduce intestinal inflammation and prevent the occurrence of some diseases by strengthening the immune system.
Even the 2019 study on Ruminococcus gnavus suggested that certain changes in a person’s diet, could slow the growth of this bacterium and perhaps reduce flares. Specifically, when there was more R. gnavus in a patient’s microbiome, there was less of another bacterium called Bacteroides uniformis. This same kind of bacteria has been shown to have anti-inflammatory properties in some studies. So, it may be possible for patients to take probiotics with microbes like B. uniformis to both control the number of “bad” R. gnavus bacteria and to limit inflammation of the gut itself.
Also, the study on Lactobacillus reuteri showed that a diet high in resistant starch, the kind that you cannot digest (as found in whole grains), can reduce the number of the “bad” L. reuteri bacteria and possibly keep them from entering the blood stream in the first place. So, there are a great many reasons to be hopeful that improving gut health through diet and perhaps probiotics can lead to improvement in the lives of those living with lupus!
Finally, studies have shown that stress can cause signals from the brain to go to the gut and increase the permeability of the intestinal walls. This can lead either bacteria or bacterial antigens to leak into the blood stream and trigger inflammation responses. So, as you prepare healthy meals, also nurture healthy emotions. Both can physically improve your gut health and hopefully limit symptoms of lupus.
.
Teri Greiling, MD, PhD, on Lupus and the Microbiome
Dr. Teri Greiling discusses her cutting edge research on the relationship between digestive health, the microbiome (the natural bacteria of the skin and digestive tract) and how they affect lupus.
.
In Conclusion
The incredibly complex ecosystem that is our gut microbiome is still an unknown frontier in medical science. It is proving to have significant effects on the health of many other systems of the body beyond the digestive tract, and in particular it is becoming increasingly linked to immunity and autoimmune diseases like lupus. As the research continues, even more relationships between our gut microbes and overall health will be found, and hopefully this will lead to future therapies and perhaps even cures!
.
References
American Museum of Natural History. (2015 November 7 – 2016 August 14). The secret world inside you [Museum exhibit]. New York, NY.
Azzouz, D., Omarbekova, A., Heguy, A., Schwudke, D., Gisch, N., Rovin, B., … Silverman, G. (2019). Lupus nephritis is linked to disease-activity associated expansions and immunity to a gut commensal. Annals of the Rheumatic Diseases, 78(7). 947-956. Retrieved from https://ard.bmj.com/content/78/7/947
Greiling, T.M., Dehner, C., Chen, X., Hughes, K., Iñiquez, A.J., Boccitto, … Kriegel, M.A. (2018). Commensal orthologs of the human autoantigen Ro60 as triggers of autoimmunity in lupus. Science Translational Medicine, 10(434) Retrieved from https://stm.sciencemag.org/content/10/434/eaan2306
Gunnars, K. (2018). Resistant starch 101 – everything you need to know. Retrieved from https://www.healthline.com/nutrition/resistant-starch-101
Minerbi, A., Gonzalez, E., Brereton, N., Anjarkouchian, A., Dewar, K., Fitzcharles, M., … Shir, Y. (2019). Altered microbiome composition in individuals with fibromyalgia. PAIN, 160(7). Retrieved from https://insights.ovid.com/crossref?an=00006396-900000000-98647
Peters, W. (2016, June). Microbiome: Gut bugs and you. [Video file]. Retrieved from https://www.youtube.com/watch?v=IDqMB6C1uys
Probiotics market size, share & trends analysis report by product (food & beverages, dietary supplements), by ingredient (bacteria, yeast), by end use, by distribution channel, and segment forecasts, 2019-2025. (2019). Retrieved from https://www.grandviewresearch.com/industry-analysis/probiotics-market
Robertson, R. (2017). Why the gut microbiome is crucial for your health. Retrieved from https://www.healthline.com/nutrition/gut-microbiome-and-health
Todar, K. (n.d.). The normal bacterial flora of humans. Retrieved from http://textbookofbacteriology.net/normalflora.html
Vanuytsel, T., van Wanrooy, S., Vanheel, H., Vanormelingen, C., Verschueren, S., Houben, E., … Tack, J. (2013). Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Neurogastroenterology, 63(8). 1293-1299.
Yang, Y., Nguyen, M., Khetrapal, V., Sonnert, N.D., Martin, A.L., Chen, H., Kriegel, M.A., & Palm, N.W. (2022). Within-host evolution of a gut pathobiont facilitates liver tanslocation. Nature, 607. 563-570. https://doi.org/10.1038/s41586-022-04949-x
Zegarra-Ruiz, D., El Beidaq, A., Iñiguez, A., Di Ricco, M., Vieira, S., Ruff, W., … Kriegel, M. (2019). A diet-sensitive commensal Lactobacillus strain mediates TLR7-dependent systemic autoimmunity. Cell Host & Microbe, 25(1). 113-127. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S1931312818305912
.
Author: Greg Dardis, MS (Updated 2022)
Professor Dardis was formerly the Chair of the Science Department at Marylhurst University and is currently an Assistant Professor at Portland State University. His focus has been human biology and physiology with an interest in autoimmunity. Professor Dardis is also the President of the Board of Directors of Kaleidoscope Fighting Lupus.
All images unless otherwise noted are property of and were created by Kaleidoscope Fighting Lupus. To use one of these images, please contact us at [email protected] for written permission; image credit and link-back must be given to Kaleidoscope Fighting Lupus.
All resources provided by us are for informational purposes only and should be used as a guide or for supplemental information, not to replace the advice of a medical professional. The personal views expressed here do not necessarily encompass the views of the organization, but the information has been vetted as a relevant resource. We encourage you to be your strongest advocate and always contact your healthcare practitioner with any specific questions or concerns.