Dealing with Dialysis While Living with Lupus
Approximately 10% to 25% of those with lupus nephritis may develop end-stage renal disease (ESRD) and require dialysis. If you have SLE and need dialysis, read on to find out what it means and how it could affect your life.
- Introduction to Lupus and Kidney Dialysis
- What is dialysis?
- What does dialysis mean for someone with lupus?
- In Conclusion
Introduction to Lupus and Kidney Dialysis
Kidneys are critical for a number of reasons, in particular – maintaining our blood’s chemical balance of salt, minerals and other electrolytes. They effectively remove toxins and harmful metabolic wastes, like urea. Without properly functioning kidneys, it is very difficult to be healthy. They also help regulate the acidity of our blood and remove excess water. Drinking too much fluid or consuming too much salt, the kidneys take keep you in balance. Kidneys are like the stabilizer on a cruise ship, ensuring that the voyage is as smooth and steady as possible even in stormy seas.
This constant balancing and filtering requires some very complex and intricate networks of blood vessels and tubules – some of the most delicate structures of the entire body. That is one reason why they can be so easily damaged.
With lupus nephritis, the kidneys may no longer work as they should. The microscopic tubes of the kidneys may become clogged or so inflamed and damaged that they are unable to filter blood effectively. As a result, the body may retain too much salt and water and in turn, blood pressure may soar. The damage may also allow glucose and protein to leak from the blood into the urine. With diabetes, this can be even worse. End-stage renal disease (ESRD) may occur when the kidneys start to shut down. If the kidneys can no longer do the job, then dialysis may be needed.
Dialysis is typically necessary for lupus nephritis when there is 50%-90% damage to the kidneys’ blood vessels and to their ability to function. At this point, a nephrologist will very likely prescribe dialysis treatment. This dialysis may be temporary if kidneys respond well to the treatment. However, if things do not improve, long-term dialysis and possibly a kidney transplant, may be necessary.
Learning about kidney damage and the possible need for dialysis, on top of having lupus, is understandably scary. While dialysis can be as life-changing as a lupus diagnosis, learning as much as you can about it can prepare you for what to expect and how to continue day-to-day life with hope.

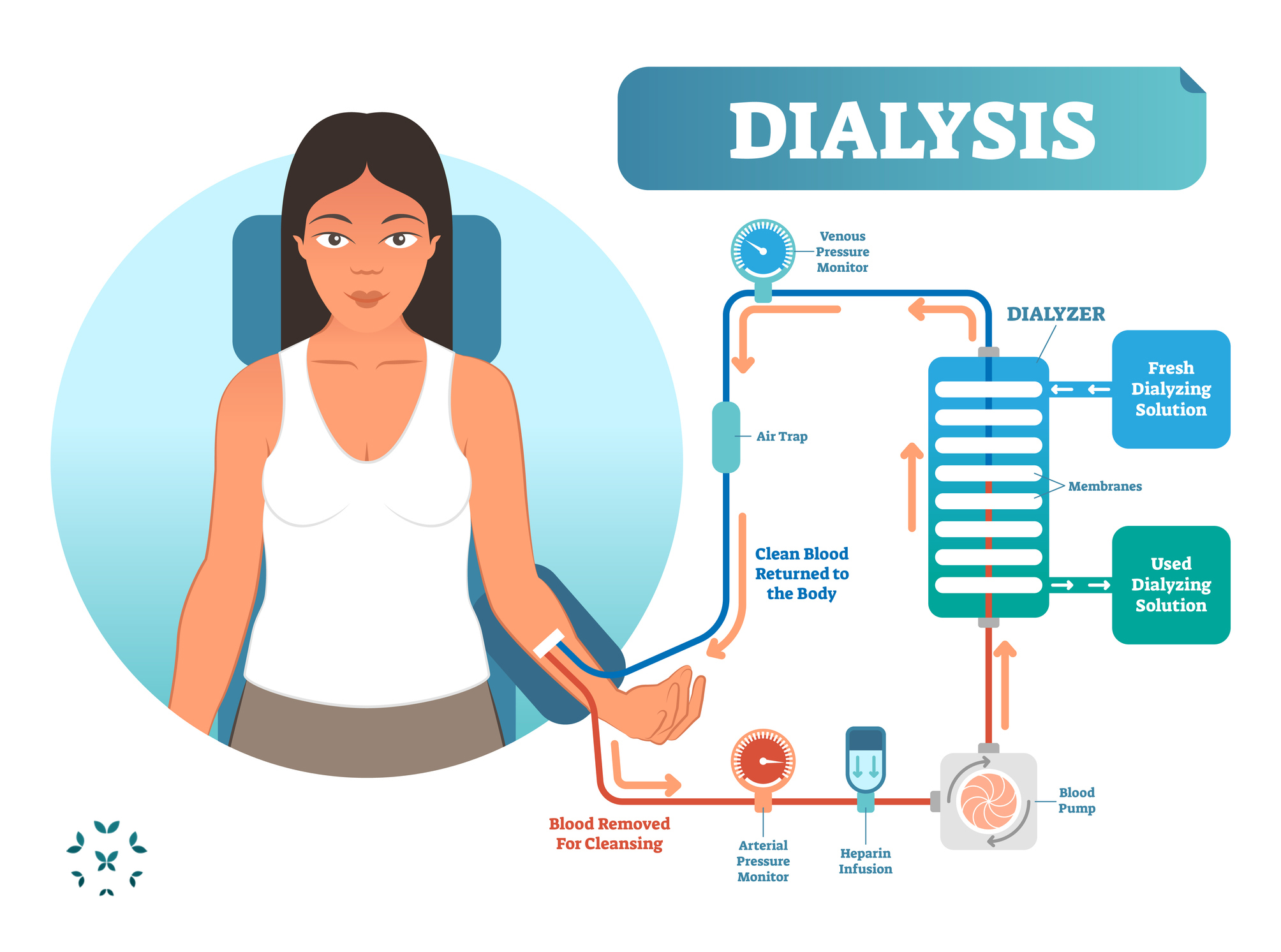
Dialysis is the filtering of blood using a machine called a dialyzer that serves as an artificial kidney. There are two main types of dialysis: hemodialysis and peritoneal dialysis. The most common is hemodialysis (HD). HD requires being hooked-up to a machine through an IV line that takes blood from a blood vessel – usually in the arm – cleans it and then returns it back into the arm. This is more complicated than it sounds, and it may require surgeries and several weeks or months to prepare the blood vessels of the arm for this process.
The dialyzer uses a fluid called dialysate containing bicarbonate, purified water, electrolytes, and minerals that removes toxins and waste from the blood through diffusion – much like the kidneys. The “clean” blood is then pumped back into the body. Each HD session lasts about five hours and may be required up to five times a week. Hemodialysis requires a expensive equipment and training, adherence to some dietary restrictions and may cause you to feel tired, with low blood pressure. However, it is efficient and is not required every day.
The second type of dialysis is called peritoneal dialysis (PD). For PD to work, a small tube or catheter is surgically placed through the peritoneum – the thin lining of the abdominal wall – and into the abdominal cavity of the body. After the dialysate enters the abdominal cavity, it fills the space and absorbs toxins and wastes from the blood as they diffuse through the peritoneal membrane itself. In this way, the peritoneum acts like a filter. Not as efficient as a kidney, but it works!
Once the dialysate absorbs enough wastes (4 – 6 hours), it passes out of the cavity, through the catheter and into a drainage bag. The used dialysate, with all of the toxins and wastes, is then discarded. Peritoneal dialysis requires dexterity and training. It is less common than hemodialysis, but it can be done without being hooked up to a lot of equipment. Also, there are fewer dietary restrictions, and it has been show to allow some patients to retain kidney function longer.
Another technique, called automated peritoneal dialysis (APD), is something of a hybrid between hemodialysis and peritoneal dialysis. The peritoneum still does the job of filtering wastes to dialysate that fills the abdomen, but a machine does the work of filling and draining the dialysate while the patient is asleep at night.
A fourth type, continuous ambulatory peritoneal dialysis (CAPD), does not require being hooked up to a machine or even to be sitting or laying down. Instead, a bag is worn over the shoulder, which fills the abdomen with dialysate by gravity. Once the dialysate has done its job, it drains out from the catheter and into another bag for disposal. This allows the patient to be able to walk around during the day. Whether APD or CAPD is used, each cycle lasts from four to five hours, and it is required most days of the week, if not daily.

Both hemodialysis and peritoneal dialysis can be done either in a clinical setting or at home. Whether or not self-care dialysis (SCD) at home is available depends on a few things:
- Does healthcare provider and clinic have the ability to deliver SCD?
- Is trained staff available?
- Is the staff able to give instructions on managing SCD?
If self-care dialysis is preferred, but not available at a particular clinic, ask to be referred to another clinic where it is available. There are some advantage of SCD, including:
- increased freedom and independence;
- lifestyle preservation;
- better adherence to treatment plans; and
- a greater feeling of control.
The healthcare team should discuss options to make sure that the best and most convenient kind of dialysis is available. It is a matter of medical need and lifestyle.
What does dialysis mean for someone with lupus?
A practitioner will generally want to get lupus to a state of low-disease activity or remission before beginning dialysis. However, if this isn’t possible, they will choose the best dialysis option – usually hemodialysis – and monitor symptoms closely. Disease activity may be high at the beginning of dialysis, but then often decreases significantly. The decrease in activity may be due to removing immune-complexes and other inflammatory factors from the lungs and blood during dialysis. It is common to be relatively free of lupus symptoms throughout the process of dialysis.
Dialysis does come with some risks for those with lupus, and these risks tend to be higher for women and those on peritoneal dialysis. Immunosuppressive therapy and dialysis do not always mix well together. Dialysis, itself, already increases the risk for infection, and taking medications that suppress the immune system, increases that risk greatly. Dialysis can increase levels of C-reactive protein (CRP) for some, which causes inflammation. Some of the more common infections that can occur include urinary tract, peritonitis (inflammation of the abdominal lining), and pneumonia. Those taking corticosteroids and other drugs such as hydroxychloroquine, will need to continue taking them until they are told otherwise by their healthcare provider.
Other risks with lupus include:
- hypertension, which is the most significant risk factor;
- diabetes;
- heart failure;
- coronary artery disease;
- peripheral arterial disease;
- cancer;
- antiphospholipid syndrome;
- blood clots; and
- reactions from PD solutions and fluid overload;
These risk factors make it crucial to follow these healthy lifestyle practices:
- quitting smoking;
- exercising as much as you are able;
- eating a heart-healthy diet and maintaining a healthy weight;
- making sure other health conditions receive treatment.
Emotional well-being is critical for maintaining good health. The whole process of dialysis can be incredibly stressful – it will take some getting used to. It is important to have a support system of people who can help when needed. Dialysis may be a time when mental health therapy would be helpful in developing good stress relief practices in order to manage any anxiety or depression that may be experienced.
Additional medications when on dialysis may include:
- blood pressure drugs;
- diuretics;
- blood thinning drugs;
- antibiotics; and
- phosphate binders to eliminate excess phosphate in the blood
Also, iron and vitamins B, C, and D are often prescribed as blood levels of these nutrients may decrease with dialysis. It is important to check with a healthcare practitioner to ensure that nothing interacts with any lupus medications already being taken. As always, communication is important!

Kidney disease and the need for dialysis can seem overwhelming and a lot to process. You probably still have a lot of unanswered questions. The best thing you can do is learn as much as you can – your life depends on it! So, for more information in the U.S., visit the National Kidney Foundation’s website at www.kidney.org. In the U.K., visit www.kidney.org.uk.
References
Chen, H., Wang, J., Chou, C., Chien, C., Chu, C., Sheu, M., Lin, Y., Chen, P., & Chien, C. (2011). Predictors of longterm mortality in patients with and without systemic lupus erythematosus: a comparative study. The Journal of Rheumatology, 38(11). Doi: 10.3899/jrheum.110311.
Common medications taken during hemodialysis. (2018). University Health Network. https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Documents/Common_Medications_Taken_during_Hemodialysis.pdf
Cucchiari, D., Graziani, G., & Ponticelli, C. (2013). The dialysis scenario in patients with systemic lupus erythematosus. Nephrology Dialysis Transplantation, 29, 1507-1513. Doi: 10.1093/ndt/gft420
Dialysis. (2021). National Kidney Foundation. https://www.kidney.org/atoz/content/dialysisinfo
Heart health: Ten tips to keep your heart healthy on dialysis. (2021). National Kidney Foundation. https://www.kidney.org/atoz/content/heart-health-ten-tips-keep-your-heart-healthy-dialysis
McLaughlin, K., Jones, H., VanderStraeten, C., Mills, C., Visser, M., Taub, K., & Manns, B. (2008). Why do patients choose self-care dialysis? Nephrology Dialysis Transplantation, 23, 3972-3976. doi: 10.1093/ndt/gfn359.
Weng, C., Hsu, C., Yu, C., Yen, T., Yang, C., & Hung, C. (2009). Peritoneal dialysis and hemodialysis in systemic lupus erythematosus patients: Comparison of clinical outcomes. Kidney Blood Pressure, 32, 451-456. Doi: 10.1159/000266480.
Author: Liz Heintz
Liz Heintz is a technical and creative writer who received her BA in Communications, Advocacy, and Relational Communications from Marylhurst University in Lake Oswego, Oregon. She most recently worked for several years in the healthcare industry. A native of San Francisco, California, Liz now calls the beautiful Pacific Northwest home.
All images unless otherwise noted are property of and were created by Kaleidoscope Fighting Lupus. To use one of these images, please contact us at [email protected] for written permission; image credit and link-back must be given to Kaleidoscope Fighting Lupus.
All resources provided by us are for informational purposes only and should be used as a guide or for supplemental information, not to replace the advice of a medical professional. The personal views expressed here do not necessarily encompass the views of the organization, but the information has been vetted as a relevant resource. We encourage you to be your strongest advocate and always contact your healthcare practitioner with any specific questions or concerns.

